It is used to prevent pregnancy.
Eileen 60 micrograms / 13 micrograms / 24 hours. transdermal patch
Gestodene / Ethinylestradiol
This product is subject to additional monitoring. This will help to quickly identify new safety information. We can help by reporting any you occurrence of side effects. For information on how to report side effects, see. End of section 4.
Important things you need to know about combined hormonal contraceptives (SHK):
- Correctly using, this is one of the most reliable reversible contraceptive methods.
- Combined hormonal contraceptives slightly increase the blood clots in the veins and arteries of the risks, especially in the first year, or re-introduction into use after 4 weeks or longer break.
- If you think you may get a blood clot symptoms, be vigilant and seek medical advice (see. Chapter 2, section "Blood clots").
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet You may need to read it.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine is only for you, so the others can not give. It may harm them.
- If you get side effects (even if it is not listed), talk to your doctor, pharmacist or nurse. See. Chapter 4.
What is in this leaflet?
- What is Eileen and what it is used for
- Before you Eileen
- How Eileen
- Possible side effects
- How to store Eileen
- Contents of the pack and other information
1. What is Eileen and what it is used for
Eileen is a patch used to prevent pregnancy.
Each patch contains two different female hormones, namely gestodene and ethinyl estradiol, which in small quantities continuously secreted by 7 days.
As Eileen contains two hormones, it belongs to the combined hormonal contraceptive group.
2. Before you Eileen
General comments
Before starting to Eileen, you must read Chapter 2 provides information about blood clots. In particular, it is important to read the symptoms of a blood clot (see. Chapter 2, section "Blood clots").
Before starting Eileen, the doctor will ask about your own and your immediate family health. In addition, the doctor will measure your blood pressure, and, depending on your state of health, may be carried out in other studies.
This leaflet describes some situations when you should stop taking or when Eileen Eileen reliability can be reduced. In such cases, you should avoid sex or use additional non-hormonal contraceptive precautions, eg., A condom or other barrier method. Do not use rhythm or temperature methods.These methods can be unreliable because Eileen changes the temperature and of the cervical mucus changes taking place during the menstrual cycle.
Eileen, like other hormonal contraceptives, does not protect against HIV infection (AIDS) or other sexually transmitted diseases.
Eileen Do not
If you have any of the following apply to you, Eileen not be used. If you have any of the following apply to you, tell your doctor. The doctor will discuss with you what would be the appropriate method of contraception.
- If you have (or have ever had) a blood clot in the legs (deep vein thrombosis, or DVT), pulmonary (lung embolism, PE) or other organs of the blood vessels;
- If you know that you have a disorder that affects blood clotting, eg., Protein C deficiency, protein S deficiency, antithrombin III deficiency, Factor V Leiden or antiphospholipid antibodies;
- if you need surgery or a long time do not walk (see section. Blood clots');
- If you have ever had a heart attack (myocardial infarction) or stroke;
- If you have (or have ever had) angina (a condition that leads to severe chest pain and may be a first heart attack [myocardial infarction] character) or transient ischemic attack (TIA - transient stroke symptoms);
- If you have at least one of the following diseases that may increase the risk of clots in the arteries:
- Severe diabetes with blood vessel damage,
- Very high blood pressure,
- Very high levels of fat (cholesterol or triglycerides) in the blood,
- A condition called hyperhomocysteinemia;
- If you are (or ever was) a certain type of migraine called "migraine with aura";
- If you have (or have ever had) liver disease (the symptoms of which may be yellowing of the skin or itching all over the body) and liver function is still impaired;
- If you have (or have ever had) cancer, which can grow in the presence sex hormones (eg., Breast or genital organs);
- If you have (or have ever had) a benign or malignant liver tumors;
- If you have vaginal bleeding of unknown cause;
- If you are allergic to ethinylestradiol or any of the other ingredients of this medicine (listed in section 6). For example, it can cause itching, rash or swelling.
If you take Eileen experience any of these conditions, immediately remove the patch, stop taking it and contact your doctor. During this period, take non-hormonal contraceptive measures. See also. See "General remarks" in Section 2 above.
Warnings and Precautions
| When should I see a doctor?
Seek immediate medical attention - If you notice a possible blood clot signs that may indicate that you have a blood clot in the leg (ie, deep vein thrombosis), blood clot in the lungs (ie, pulmonary embolism), heart attack (myocardial infarction) or stroke (see. Section "Blood clots (thrombosis) below). The serious side effects are described in the section "How to recognize a blood clot.
|
Check with your doctor, pharmacist or nurse before taking Eileen.
In some cases, Eileen, or any other combination hormonal contraceptive should be used with extreme caution, and your doctor may need to regularly tested.
If any one of the following apply to you, tell your doctor. If this condition occurs, or difficulty taking Eileen, also you need to tell your doctor.
- If you smoke;
- If you have diabetes;
- If you are overweight;
- If you have high blood pressure;
- If you have a heart condition (valve disorder, a heart rhythm disorder);
- If someone else in your blood relatives ever had a blood clot (thrombosis in the leg, lung (pulmonary embolism) or other organs), heart attack (myocardial infarction) or stroke at an early age;
- If you suffer from migraines;
- If you have epilepsy (see. Section "Other medicines and Eileen" in Chapter 2);
- If a close relative in your blood is (or ever had) breast cancer;
- If you have liver or gallbladder disease;
- If you have depression;
- If you suffer from Crohn's disease or ulcerative colitis (chronic inflammatory bowel disease);
- If you suffer from systemic lupus erythematosus (SLE - disease that affects the body's natural defense system);
- If you have haemolytic uraemic syndrome (HUS - kidney failure resulting in blood clotting disorder);
- If you have sickle cell anemia (an inherited disease of red blood cells);
- If you have high blood fat levels (hypertriglyceridaemia) or a positive family history of this condition. Hypertriglyceridemia is associated with an increased risk of pancreatitis (inflammation of the pancreas) development risks;
- If you need surgery or a long time do not walk (see. Section 2 'Blood clots');
- If you have just given birth, you are at increased risk of blood clots. Ask your doctor how long after birth, you can start by Eileen;
- If you have inflammation of the subcutaneous vein (superficial thrombophlebitis);
- If your veins knotty and enlarged;
- If you have a condition that first appeared or worsened during pregnancy or previous use of sex hormones at the time (eg., Decreased hearing, metabolic disease called porphyria, a skin disease called herpes gestationis, or Sydenham's chorea - nerve disease causing sudden body movements;
- If you have (or ever was) yellow-brown pigmented spots (also known as "pregnancy patches"), especially on the face (chloasma) In this case, avoid direct exposure to sunlight or ultraviolet rays;
- If you have hereditary angioedema. If you experience symptoms of angioedema (swelling of the face, tongue, or (or) and throat (or) difficulty swallowing or hives together with difficulty in breathing), contact your doctor immediately. Medications containing estrogen may cause or exacerbate symptoms of angioedema.
Blood clots
Combination hormonal contraceptive, such as., Eileen, you have a higher blood clot risk than without using it. In rare cases, a blood clot can block the blood vessels and lead to serious disturbances.
Blood clots can occur
- veins (known as venous thrombosis, venous thromboembolism or VTE)
- arteries (called arterial thrombosis, arterial thromboembolism or ATE).
Blood clots are not always completely disappear. In rare cases, blood clots can cause serious long-term consequences, or in very rare cases, they can be fatal.
It is important to remember that the overall harmful blood clot due to Eileen consumption is low.
How to recognize a blood clot
If you notice any of these signs or symptoms, seek immediate medical attention.
| Do you experience any of these symptoms? | What you may have the condition? |
|---|---|
| · One leg, foot swelling, or swelling along the leg veins, especially if associated with: · Leg pain or soreness, which can be felt only when standing or walking; · Affected leg elevated temperature; · Abnormal, eg., Pale, red or cyanotic leg skin color. | Deep vein thrombosis |
| · Sudden unexplained shortness of breath or breathing; · Sudden coughing for no apparent reason, which may be bloody; · Sharp chest pain, which may increase deep breathing; · Severe dizziness or vertigo; · Fast or irregular heartbeat; · Severe stomach pain.
If in doubt, ask your doctor, because some of these symptoms, eg., Coughing or shortness of breath may be incorrectly easier to maintain state, for example., Respiratory tract infection (eg., A cold).
| Pulmonary embolism |
| Symptoms usually occur in one eye: · Sudden loss of vision or · Pain does not cause blurred vision, which can progress to blindness
| Retinal vein thrombosis (blood clot in the eye) |
| · Chest pain, discomfort, pressure, heaviness; · Tightness or feeling of fullness in the chest, arm or under the breastbone; · Fullness, indigestion or choking feeling; · Upper body discomfort radiating to the back, jaw, throat, arm and stomach; · Sweating, nausea, vomiting or dizziness; · Very big weakness, anxiety or shortness of breath; · Fast or irregular heart beat.
| A heart attack (myocardial infarction) |
| · Sudden the face, arm or leg numbness or weakness, especially on one side of the body; · Sudden confusion, speech or understanding of the disorder; · Sudden vision in one or both eyes disorder; · Sudden difficulty walking, dizziness, balance or coordination problems; · Sudden, severe or prolonged headache without a known cause; · Loss of consciousness or fainting with or without seizure.
Sometimes the symptoms of stroke may be short-term, and they can almost instantly and completely disappear, but you still need to seek emergency medical help, because you can be the next stroke.
| stroke |
| · Swelling of limbs and light blue discoloration; · Severe abdominal pain (acute abdomen). | Blood clots that obstruct blood vessels in other
|
Blood clots in a vein
What can happen if a blood clot in a vein?
- Combined hormonal contraceptive use is associated with an increased risk of blood clots in a vein (venous thrombosis). However, these side effects are rare. Most often it occurs in the first combined hormonal contraceptive use year.
- If the leg or foot vein blood clot, it can lead to deep vein thrombosis (DVT).
- If a blood clot from the legs to the lungs, it can cause a pulmonary embolism.
Very rarely, blood clots can form another body, for example., Eye vein (retinal vein thrombosis).
When a blood clot in a vein at highest risk?
The maximum blood clot in the vein, the risk is in the first year, the combined hormonal contraceptive is used for the first time. These risks may also be higher, if the re-start combined hormonal contraceptives (the same or a different medicine) after 4 weeks or longer break.
After the first year, this risk is decreasing, but is slightly higher than without the use of a combined hormonal contraceptive.
Upon termination of Eileen use you in the risk of blood clot returns to normal within a few weeks.
What is the risk of blood clots?
This risk depends on you the natural risk of VTE and used the combined hormonal contraceptive type.
General blood clot in the leg or lung (DVT or PE) risk associated with Eileen is low.
- Approximately 2 out of 10 000 women who are not receiving the SHK is not pregnant within a year the blood clots.
- Approximately 5-7 per 10 000 women who use combined hormonal contraceptives containing levonorgestrel, norethisterone or norgestimate, during the year, the blood clots.
- Approximately 9-12 per 10 000 women who use combined hormonal contraceptives containing gestodene, eg., Eileen, during the year, the blood clots.
- Is not yet known what the risk of blood clots taking Eileen, compared to the risk associated with combined hormonal contraceptive containing levonorgestrel and combined oral contraceptives containing gestodene.
- Risk of blood clots is varied and depends on the individual medical history (see. "Factors that increase the risk of blood clot" below).
|
| Blood clot in a year, the risk of |
|---|---|
| Women who do not use combined hormonal pill, patch or ring and not pregnant | About 2 out of 10 000 women |
| Women who take combined hormonal pills containing levonorgestrel, norethisterone or norgestimate | Approximately 5-7 out of 10 000 women |
| Women who are taking combined oral contraceptives containing gestodene. | Approximately 9-12 out of 10 000 women |
Factors that increase the risk of blood clots in the veins
Blood clot risk associated with Eileen is small, but some condition that increases the risk. This risk is higher:
- If you have a lot of excess weight (body mass index (BMI) over 30 kg / m 2 );
- If any of your blood relatives had a blood clot in the leg, lung or other organ at an early age (eg., Up to about 50 years). In this case, you may have an inherited blood clotting disorder;
- If you need surgery or do not walk for a long time due to injury, illness or legs in plaster. A few weeks before surgery or until your mobility is limited, you may need to stop taking Eileen. If you need to stop treatment with Eileen, ask your doctor when you can start again to use it;
- With age (especially if you have more than about 35 years old);
- Have given birth less than a few weeks.
The more of these conditions apply to you, at the risk of blood clots is higher.
Travelling by air (> 4 hours) may temporarily increase the risk of blood clots, especially if you have other risk factors listed.
It is important to tell your doctor if you fit any of these conditions, even if you are not sure. Your doctor may decide that Eileen should be discontinued.
If you take Eileen changed any of the conditions listed above, eg., Blood relative thrombosis occurred without a known cause or gain a lot of weight, tell your doctor.
Blood clots in arteries
What can happen if a blood clot in an artery?
Arteries, as well as vein, a blood clot can lead to serious complications. For example, it can cause a heart attack (myocardial infarction) or stroke.
Factors that increase the risk of a blood clot in an artery
It is important to note that the risk of heart attack (myocardial infarction) or stroke for Eileen consumer risk is very small, but it can be increased:
- Age (over about 35 years of age);
- If you smoke. The use of combined hormonal contraceptives, eg., Eileen, it is advisable not to smoke. If you are unable to quit smoking, and you are more than 35 years old, your doctor may advise you to use another method of contraception;
- If you are overweight;
- If your blood pressure is elevated;
- If any of your blood relatives had a heart attack (myocardial infarction) or stroke at an early age (around 50 years). In this case, you can also be higher heart attack (myocardial infarction), or stroke;
- If you or anyone in your immediate family, found high levels of fat (cholesterol or triglycerides) in the blood;
- If you suffer from migraine, particularly migraine with aura;
- If you have a heart condition (valve disorder or arrhythmia called atrial fibrillation);
- If you have diabetes.
If you to more than one of the following conditions, or any of these conditions is a serious risk of blood clots may be even greater.
If you take Eileen changed any of the conditions listed above, eg., Started smoking, blood relative thrombosis occurred without a known cause or gain a lot of weight, tell your doctor.
Combined hormonal contraceptives and cancer
Combined hormonal contraceptives in women taking a little more determined breast cancer, but is not known whether it is caused by the same treatment. Eg., Maybe women who take combined hormonal contraceptives are often the doctor examined so tumors diagnosed more frequently. Upon termination of the combined hormonal contraceptive, the risk of breast tumors diminishing. It is important to regularly check the breasts and deducing any lump, contact your doctor.
In rare cases in users of combined hormonal contraceptives for women to identify benign liver tumors, and even more rarely - malignant liver tumors. In isolated cases, these tumors have led to life-threatening internal bleeding. If you have unusual severe abdominal pain, see your doctor.
The primary cervical cancer risk factor is the Persistent human papillomavirus (HPV) infection. Some studies suggest that long-term use of combined hormonal contraceptives increase the risk of developing cervical cancer. Still, it is unclear how much this increases the risk of sexual lifestyle or other factors, for example., The human papilloma virus.
Bleeding between menstrual
As with all combined hormonal contraceptives, the first few months may be irregular vaginal bleeding (spotting or cause Bleeding between periods) between menstruation. You may need to hygiene measures, but continue to take Eileen as usual.
The body adapts to Eileen, irregular vaginal bleeding usually disappear (usually after about 3 cycles of treatment). If it persists, abundant, or starts again, tell your doctor.
What to do if no bleeding
If Eileen taken properly and not taken any other drugs are not likely to become pregnant. Take Eileen continue as usual.
If Eileen taken improperly or if Eileen taken properly, but the bleeding does not happen twice in a row, you may be pregnant. Contact your doctor immediately. Do not start the next patch until you are sure that you are not pregnant. During this period, take non-hormonal contraceptive measures. See also. See "General remarks", above, in Section 2.
Children and adolescents
Eileen safety and efficacy of adolescents under 18 years of age have not been established.
Other medicines and Eileen
If you are taking or have recently taken any other medicines or herbal products, including medicines obtained without a prescription, or because you are not sure, talk to your doctor or pharmacist. Also tell any other doctor or dentist who prescribes another medicine (or the medicines issued the pharmacist) that you are taking Eileen. They will be able to tell you if you need to use an additional contraceptive method (eg., A condom) and, if appropriate, of the time to use them, or to advise whether it is necessary to change the other medicines you may require.
Some medicines can act Eileen blood and weaken its effectiveness in protecting against pregnancy, or can cause unexpected bleeding. These include:
and drugs used to treat these conditions:
- Epilepsy (eg., Primidone, phenytoin, barbiturates, carbamazepine, oxcarbazepine,
eslicarbazepine, topiramate, felbamate);
- Tuberculosis (eg., Rifampicin, rifabutin)
- Sleep disorder narcolepsy (modafinil);
- High blood pressure in the lungs (bosentan);
- HIV and hepatitis C virus infections (so-called protease inhibitors and non-nucleoside reverse transcriptase inhibitors), other infections (griseofulvin);
and herbal preparation St. John's wort.
Combined hormonal contraceptives may have an effect on other medicines, eg., Anti-epileptic lamotrigine.
Labaratory tests
If you need a blood test or other laboratory tests, tell your doctor or laboratory staff that you are taking Eileen, because hormonal contraceptives can affect the results of some tests.
Eileen with food, drink and alcohol
It is unlikely that food, beverages or alcohol would affect the functioning of Eileen.
Pregnancy and breast-feeding
If you are pregnant or think you may be pregnant, Eileen not be used. If you become pregnant while taking Eileen, immediately remove the patch and call your doctor.
If you want to get pregnant, you can stop by Eileen use at any time (see also. See "If you stop taking Eileen" in Chapter 3).
Usually Eileen breast-feeding is not recommended. If you want to use Eileen breast-feeding, you should seek medical advice.
Driving and using machines
Taking Eileen can drive or operate machinery.
3. How Eileen
Always take this medicine exactly as directed by your doctor or pharmacist. If in doubt, talk to your doctor or pharmacist.
Eileen prevents you from getting pregnant, because through the skin into your body falls hormones.For the patch to work properly, it must be good to stick to the skin.
Eileen effectiveness depends on how you are following the instructions for use of the patch. The more closely you follow these instructions, the less likely that you are pregnant.
So Eileen always exactly as described in the brochure. Failure to follow these instructions may increase the chances of pregnancy.
When did you first start taking Eileen
Mark the day of the week stuck on the first patch. The day of the week will be your patch change day every week (see also. See "patch" Change Day "in Section 3 below).
Follow the rules as to the use of Eileen, or how to replace the previous method of Eileen consumption.Last month, the contraceptive method used to select the left column of the table below:
Rules as to the use of Eileen, or how to replace the previous method of use Eileen
| Last month, the used method of contraception | Rules as to the use of Eileen, or how to replace the previous method of use Eileen
|
|---|---|
| Hormonal contraceptives without prior treatment | Start taking Eileen on the first day of the cycle (1st day of menstruation). Eileen will take effect immediately, additional contraceptive method is required.
The patch can be sealed and 2-5 of the cycle time, but then, after sticking the first patch, 7 days will need to use an additional contraceptive method (eg., A condom). |
| Combined hormonal contraceptive tablets | We recommend that you start by Eileen day after administering the last hormone-containing pills in the pack. This means that the tablets are not a break. If your tablets are hormone pills do not, you can start by Eileen day after administering the last tablet containing hormones. If in doubt, which is a tablet, ask your doctor or pharmacist.
The patch can be started at a later date, but no later than the first day after the end of pill-break (or the first day after administering the last hormone-free pill). |
| Combined contraceptive vaginal ring | Start taking the last cyclical Eileen pack ring removal day, but not later than it should be the next use.
|
| Combined contraceptive patch | Start taking Eileen last cyclical package patch removal day, but not later than it should be the next use.
|
| Progestogen-only pills (low dose birth control pills) | These pills can change Eileen any day without a break.
Sticking the first patch, 7 days will need to use an additional contraceptive method (eg., A condom).
|
| Progestogen implant | Start taking Eileen implant removal day.
Sticking the first patch, 7 days will need to use an additional contraceptive method (eg., A condom).
|
| Progestogen-releasing intrauterine system | Start taking Eileen the day of removal.
Sticking the first patch, 7 days will need to use an additional contraceptive method (eg., A condom).
|
| Progestogen-only injection | Eileen Start taking the next injection.
Sticking the first patch, 7 days will need to use an additional contraceptive method (eg., A condom). |
After a miscarriage
Follow your doctor's advice.
After giving birth
If you just had a baby, your doctor may tell you to wait for the first normal menstrual period and then start Eileen. Sometimes it is possible to start sooner. Your doctor will advise you.
If after the birth before taking Eileen already had sex before užsiklijuodama patch, you must make sure you are not pregnant or wait for the first normal menstruation.
If, after giving birth to begin the use of Eileen and breast-feeding, discuss this with your doctor.
If you are not sure when to start Eileen, talk with your doctor what to do.
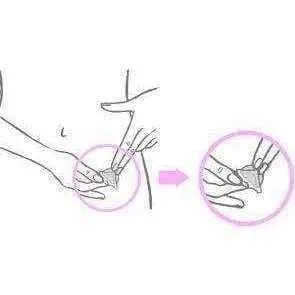
Where to stick the patch
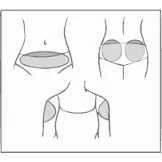
Apply Eileen only in these areas: the abdomen, buttocks or upper part of the upper arm, where the patch will not be rubbed by tight clothing (see. Fig. Below). For example, attach the patch at the waist clothes.
Make sure that the skin at the application site is intact, sound, clean, dry and - preferably - hairless.Do not stick the patch on the breast, on the cut, red or irritated skin or in the same place where it glued the last time.
In the area of the skin where there is or will be sealed Eileen, do not use lotions, creams, oils, powders or powder, make-up or other topical products. This could keep the patch from sticking or part of it may become loose.
Change the patch application, using the same bonding different field locations. For example. You can change the application site from the left side of the abdomen to the right or left side of the buttocks or upper arm to the right.
In addition, you can stick every week in a different location (eg., One week in the outer part of the upper arm, next week - on the stomach).
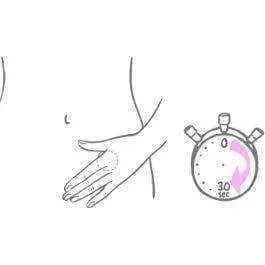
Every day and check that the patch firmly stuck to the skin.
Please note
- At the same time, take only one patch.
- If the patch is worn properly, you can bathe or shower as usual.
- If the patch remains properly adhering, no restrictions, eg., You can swim, sunbathe sauna and sports.
- A clear patch is protected from ultraviolet radiation of sun light so it can be exposed to solar radiation and need not be covered by clothing.
What do you receive in a pharmacy
Eileen pharmacy received a box containing the leaflet and 3, 9 or 18 sealed sachets, each containing one Eileen patch.
Sachets depends on the prescription that you get the prescription the doctor.
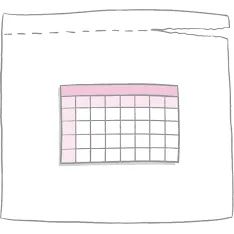
Each sealed sachet contains one patch to stick to the skin. The patch is round and clear:
- The adhesive side of the patch is covered with two pieces of square-glossy, transparent protective film.
- On the opposite side of the patch is covered with a white, square-shaped coating, which prevents the patch from sticking to the internal sachet.
| Round, transparent patch |
| White, |
How to prepare a patch
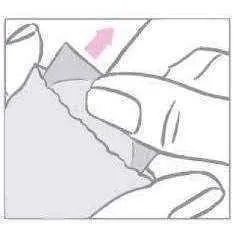
- Use your fingers to tear the top of the sachet. Where looting indicates notches.
Do not use scissors. Do not cut, not to damage or otherwise alter the patch, as this may weaken its contraceptive effect.
- Round contraceptive patch is between the two parts of the square-shaped shiny, transparent protective films and a white square of the cladding layer. It is important to remove the patch from the sachet together with a transparent protective film and a white coating. Do not discard the sachet. Sachet need to stay pavartotam patch handle (see. Section patch management "in Chapter 5).
- After opening the sachet, the patch should be applied immediately stick, as described below.
- First of all, from the upper part of the patch remove one part white square covering layer.
After removing from the patch of white square covering layer, which prevents the patch from the inside sticking to the sachet, this layer should be discarded.
Two-piece square glossy transparent protective film covers a round, transparent patch bottom (adhesive) part. Adhesive side are active drugs. Avoid touching the sticky surface of the patch that he remained sticky.
- Then pee